Background: High expression of the very late antigen-4 (VLA-4) integrin subunit CD49d predicts disease progression in chronic lymphocytic leukemia (CLL). We previously demonstrated that B cell receptor (BCR) signals induce activation of VLA-4 (Tissino et al., J Exp Med. 2018) and characterized Eµ-TCL1-transgenic (TCL1-tg) mice as an adequate model for the human high-risk CD49d-high CLL patient subgroup, with VLA-4 inhibition hampering the disease (Szenes et al., Leukemia 2020). Here, we address the consequences of genetic B cell-specific ablation of CD49d on disease development, engraftment capacity and treatment susceptibility in a novel CLL mouse model.
Methods: We crossed ITGA4fl/fl mice, kindly provided by T. Papayannopoulou, University of Washington, with TCL1-tg mice and CD19 Cre mice, subsequently named CD49d∆B TCL1-tg. Tumor development was continuously monitored by regular blood checks and mice were sacrificed at 10 months. Tumor infiltration was quantified in peritoneal cavity (PC), spleen and bone marrow by flow cytometry using anti-CD5/CD19 antibodies. Integrin and chemokine receptor expression was profiled. In vitro responsiveness to BCR stimulation of CD49d-deficient and proficient leukemic cells was assessed using phospho-specific flow cytometry. Furthermore, purified leukemic cells derived from PC or spleen were subjected to RNA-seq analyses. CD49d-deficient or proficient leukemic cells were transplanted into wild-type C57BL/6J recipients in short and long term experiments. Ongoing: CD49d-deficient or proficient leukemic cells were transplanted competitively into C57BL/6J recipients and are receiving continuous Bruton's tyrosine kinase (BTK)-inhibitor (acalabrutinib) treatment upon tumor onset.
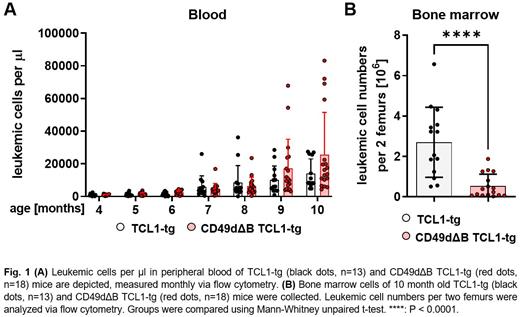
Results: CD49d∆B TCL1-tg mice showed a B cell-specific integrin loss in all organs. Blood tumor burden was measured monthly. At months seven and eight, leukemic cells of CD49d∆B TCL1-tg mice were reduced by approx. 25% compared to TCL1-tg littermates (Fig. 1A). This trend was reversed at month nine, with approx. 45% increased lymphocytosis in CD49d∆B TCL1-tg mice. CD49d expression in leukemic cells of TCL1-tg mice was unaffected by disease progression. At sacrifice, CD49d∆B TCL1-tg mice showed an 80% ( p=<0.0001) reduction of tumor burden in the bone marrow (Fig. 1B), but comparable leukemic cell numbers in PC and spleen.
Leukemic splenocytes derived from CD49d∆B TCL1-tg mice displayed 38% ( p=0.032) higher IgM and 33% higher CD44 expression but 43% ( p=0.015) reduced expression of CXCR4. BCR signaling was modulated by the integrin loss and BCR stimulation with anti-IgM induced 43% ( p=0.022) higher PLCγ2 and 45% ( p=0.022) higher SYK phosphorylation in leukemic cells derived from CD49d∆B TCL1-tg mice compared to littermates, but comparable BTK phosphorylation.
RNA-seq analysis revealed strong differences in leukemic cell transcriptomes between PC and spleen, indicating tissue dependent effects on leukemic cells. Particularly, TNF-α signaling via NF-κB, MTORC1, MAPK signaling and JAK-STAT signaling pathways were upregulated in leukemic cells derived from spleen compared to PC irrespective of CD49d expression, while chemokine signaling pathways were downregulated in PC. When comparing CD49d deficient and proficient leukemic cells, the gene set MYC targets v1 was enriched in deficient cells.
When injecting CD49d-deficient leukemic splenocytes intravenously, more cells were recovered after 5 days from blood ( p=0.048) and spleen compared to CD49d-proficient cells, but did not engraft in bone marrow or peritoneum. When injected intraperitonally, CD49d-deficient leukemic cells were found in peritoneum in contrast to TCL1-tg littermates ( p=<0.0001).
Conclusion: The TCL1 mouse model resembles a human high-risk CLL (e.g. IGHV unmutated, CD49d-expressing), and thus allows to investigate the impact of CD49d expression in this CLL subset. Loss of CD49d expression resulted in an altered redistribution of leukemic cells in tissue sites with a significant reduction of leukemic cells in the bone marrow. Lack of integrin signals resulted in increased antigen-induced BCR signaling and IgM expression, as well as a B cell receptor activation phenotype associated with MYC gene set enrichment, indicating a feedback loop from integrins to the BCR. Currently, the susceptibility of CD49d∆B TCL1-tg mice to BTK inhibitors is under investigation.
Disclosures
Polcik:AstraZeneca: Research Funding. Greil:Roche: Honoraria, Research Funding. Shoumariyeh:Blueprint: Consultancy; BMS: Speakers Bureau; Astrazeneca: Honoraria; Novartis: Honoraria. Duque Afonso:SOBI: Honoraria, Other: Travel Support; Riemser: Honoraria; Amgen: Honoraria; Roche: Consultancy, Honoraria, Other: Travel Support; IPSEN: Honoraria; NovoNordisk: Honoraria; AstraZeneca: Honoraria; Roche: Other: Travel Support; Lilly: Other: Travel Support. Hartmann:AstraZeneca: Research Funding.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal